CMS Releases 2026 Medicare Home Health Prospective Payment System Final Rule

CMS Releases 2026 Medicare Home Health Prospective Payment System Final Rule
 The Centers for Medicare & Medicaid Services (CMS) has released the Calendar Year (CY) 2026 Home Health Prospective Payment System (PPS) final rule, a wide-ranging regulation that updates Medicare home health payment rates and implements numerous policy, quality reporting, and program integrity changes. These regulations take effect on January 1, 2026.
The Centers for Medicare & Medicaid Services (CMS) has released the Calendar Year (CY) 2026 Home Health Prospective Payment System (PPS) final rule, a wide-ranging regulation that updates Medicare home health payment rates and implements numerous policy, quality reporting, and program integrity changes. These regulations take effect on January 1, 2026.
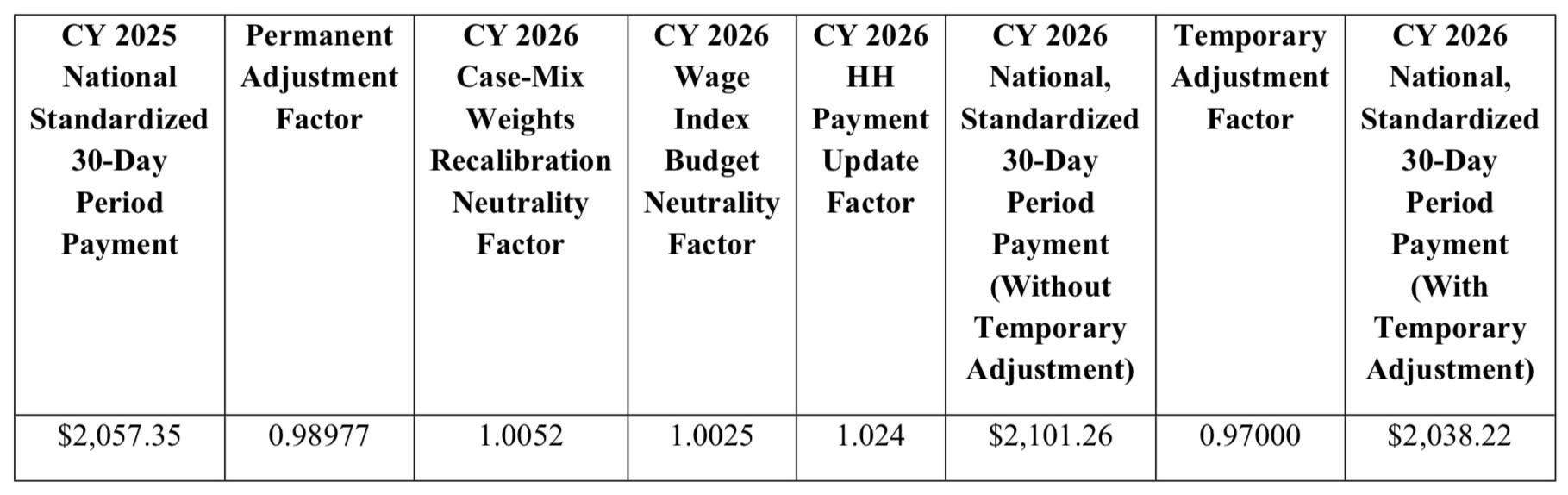
While CMS originally proposed a significant permanent payment reduction of approximately $60 per 30-day period, the final rule instead adopts a much smaller — but still impactful — net decrease of approximately $19 per 30-day period, once all permanent, temporary, and technical adjustments are combined. This reflects CMS’s recalculation of assumed versus actual behavior changes under the Patient-Driven Groupings Model (PDGM) using updated 2024 data.
Overall, CMS estimates a $220 million (-1.3%) decrease in aggregate Medicare payments to home health agencies for CY 2026. These regulations are effective on January 1, 2026.
Key Provisions
Payment Rate & PDGM Adjustments
- A -1.023% permanent adjustment and a -3.0% temporary adjustment for CY 2026.
- Updated case-mix weights, functional impairment levels, comorbidity groupings, and Low-Utilization Payment Adjustment (LUPA) thresholds.
- The finalized reductions equal approximately $19 per 30-day period, substantially less than the originally proposed ~$60 cut.
Home Health Quality Reporting Program (HH QRP)
- Removal of the COVID-19 vaccination measure and four standardized patient assessment data elements.
- Implementation of a revised Home Health Consumer Assessment of Healthcare Providers and Systems (CAHPS®) survey beginning April 2026.
- Updated reconsideration and extraordinary-circumstance exception processes.
Home Health Value-Based Purchasing (HHVBP) Model
- Removal of three CAHPS®-based measures.
- Addition of four new measures, including the claims-based Medicare Spending per Beneficiary – Post-Acute Care (MSPB-PAC) measure and three OASIS-based self-care functional measures related to bathing and dressing.
- Revisions to weighting across measure categories.
Conditions of Participation (CoPs)
- Technical updates clarifying that OASIS reporting applies to all skilled patients, regardless of payer.
Provider Enrollment
- Expanded grounds for denial, revocation, and deactivation.
- Mandatory reporting of adverse legal actions shortened from 90 days to 30 days.
- Expanded authority for retroactive effective dates.
For a detailed breakdown of the final rule, click here to read the comprehensive analysis from the National Alliance for Care at Home.